Faced with surgical challenges presented by the COVID-19 pandemic, the Providence Breast Centre at Mount Saint Joseph Hospital seized the opportunity to expand the use of a technique called regional anesthesia. The results: shorter hospital stays, less pain for patients, an increased number of breast surgeries and lower risk of virus exposure.
No breathing tube needed for local anesthetic
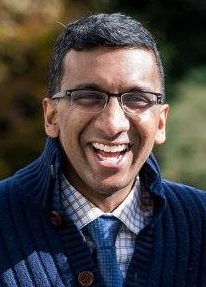
“Because COVID-19 is spread by aerosol droplets, inserting a breathing tube for a general anesthetic increases the risk of exposure for staff in the operating room,” says Dr. Chris Prabhakar, Director, Regional Anesthesia, Providence Health Care. “As well, initial COVID-19 guidelines suggested that we needed to wait upwards of 20 minutes to allow the air to safely exchange before we could open the doors to the OR. This meant that every surgery requiring general anesthesia took 40 minutes longer.”
While critical to mitigating the spread of COVID-19, these new guidelines reduced the number of breast surgeries the team could perform. They knew they needed other options to ensure their patients received care in a timely manner.
Going from nurse to patient
“It was surreal, sitting in my doctor’s office and hearing him tell me my biopsy results,” recalls Holly Andrews, diagnosed with breast cancer last September.
A registered nurse and the clinical nurse leader in the cardiology unit at St. Paul’s Hospital, Andrews was healthy and active. The news of her diagnosis was a shock for her and her close-knit family.
“It was scary to be the patient, not the health-care provider. I hadn’t had surgery in decades and I didn’t know what to expect,” says Andrews. “It all happened very quickly. I was scheduled for surgery two weeks after I found out I had breast cancer.”
Public health orders meant that she could not have all of her family physically around as she coped with her diagnosis and impending surgery. In particular, she missed her nephew, Levi.
No need for breathing tube
Fortunately for Andrews, the team at Providence Breast Centre had implemented a technique called a peripheral nerve block. It uses local anesthesia (like the kind your dentist gives you before a filling) that is injected as a regional anesthetic in the back and chest to numb the breast area. There is no need for loss of consciousness, paralysis, or a breathing tube as with a general anesthetic.
Pre-pandemic, a handful of anesthesiologists were able to administer this type of nerve block. When the pandemic hit, the team realized it could lower the risk of COVID-19 transmission and reduce the amount of personal protective equipment health-care workers needed. What’s more, patients who have a nerve block recover more quickly and report less pain after surgery than patients who receive a general anesthetic.
Regional anesthesia specialists within the department quickly became adept at performing these blocks. Soon, the team had a dozen anesthesiologists who could administer these nerve blocks, allowing them to offer this option on a daily basis.
A nerve block takes about 20 to 30 minutes to work once it is injected. One anesthesiologist was dedicated to administering the nerve block outside the operating room while other members of the team were operating on another patient.
Discharged an hour after surgery
“When I met with my anesthesiologist pre-surgery, he offered the nerve block as an option,” Andrews says. “I was really impressed. I was awake immediately following my surgery and very comfortable. I was able to go home about one hour later.”
“Pain management after surgery is better than with general anesthesia. The pain medications used after general anesthesia often have unwanted side effects, like nausea and respiratory depression,” says Dr. Prabhakar. “After nerve blocks, patients have a lower risk of nausea and vomiting, and fewer respiratory issues. This means that they feel better and are able to leave the hospital sooner.”
In fact, some patients having total mastectomies and breast reconstruction, which traditionally cause enough pain to warrant overnight admission to hospital, were being discharged home the same day.
“Patients often feel better recovering at home, and there is also a cost-saving for the health system if they don’t stay overnight,” he continues. “In addition, using regional anesthesia means that we can provide more surgeries by decreasing anesthesia time and waiting time in the OR.”
Patients like the nerve block
Eighty-six per cent of patients surveyed were happy with the nerve block and it is quickly gaining popularity. In 2019, only three per cent of patients had regional anesthesia for breast surgeries. That number quickly grew in 2020 and today, 89 per cent choose a nerve block.
“Following my initial lumpectomy, I was told that I needed to have a second surgery to remove some more tissue and to assess my lymph nodes,” says Andrews. “I requested a nerve block, given how well it worked for me the first time.”
Andrews had no complications from her second surgery and after two weeks she was able to return to the work that she loves.
“I am so grateful. Everyone I dealt with was so professional, kind and caring,” Andrews says. “You do not know what to expect going in and it is amazing to realize that something like this can end in a positive experience.”
“Given all of these positive benefits for patients and health care providers,” says Dr. Prabhakar, “the nerve block process is very likely a permanent addition to the surgical program at Mount Saint Joseph.”





