Eating Disorder Awareness Week (EDAW) is February 1 to 7. This national week of action is focused on educating the public about eating disorders.
Have you ever had your feelings invalidated? Perhaps you were told you were overreacting or that you shouldn’t feel the way you do about something. Imagine that happening when you’re seeking help from a health care provider.

“People who have an eating disorder find it unhelpful to be pushed to make changes until they’re ready and want to,” said Dr. Geller, associate professor in the UBC Department of Psychiatry. “People recall being told to ‘just eat’ or ‘just don’t eat,’ as if it’s that simple. Care providers need to understand that eating disorders happen for a reason and that they are difficult to change. That’s why validation and compassion are so important. They help the individual feel like they’re not alone, they’re understood, and they have some agency over their treatment.”
The Power of Feeling Seen
Recently published research from Dr. Geller and her colleagues at UBC and St. Paul’s Hospital took a deep dive into how important validation really is.
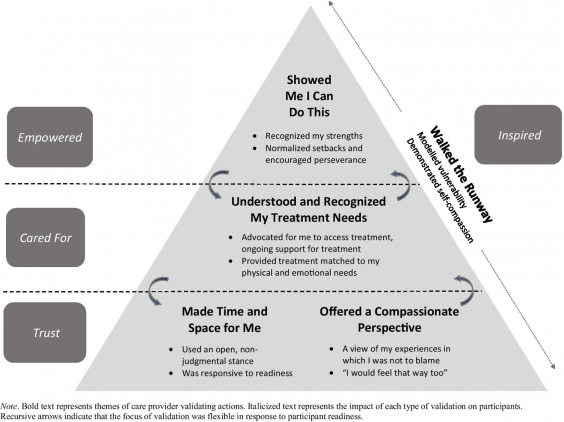
Speaking with 18 people who were in recovery or had recovered from an eating disorder, the ‘Power of Feeling Seen’ project identified five care provider actions that helped patients feel validated:
- Making time and space for the individual
- Offering a compassionate perspective
- Understanding and recognizing the individual’s treatment needs
- Showing the individual that they can make changes
- Walking the runway (care providers demonstrating that they practice self-compassion)
These actions were in turn associated with patients feeling trust, cared for, empowered, and inspired.
As demonstrated in the image below, the impacts of validating experiences build upon one another and can change depending on the patient’s circumstance or readiness. It is common to encounter hurdles that require different levels of validation. As such, it is important that care providers are flexible, allowing a shift in the focus of their actions and switching up the level of validating care they provide.
For Psychology Month, Dr. Geller’s team developed a flyer describing the levels of validation and their impact on patients’ experiences. It also details how friends, family, colleagues, and teachers can make a difference by providing validation.
The importance of self-compassion
Self-compassion means that when you face a problem, instead of being harsh with yourself, you treat yourself with the same kindness and understanding you would treat a valued friend. It involves a sensitivity to one’s suffering with a commitment to try to alleviate and prevent it.
“Self-compassion is a vital part of the eating disorder recovery journey. We found that overcoming barriers to self-compassion was associated with greater benefit from treatment,” explained Dr. Geller.
Dr. Geller is currently developing a new five-session intervention that targets readiness for self-compassion. The hope is that this new intervention will decrease barriers to patients’ practice of self-compassion.
A recommendation for health care providers
If there’s one thing that care providers should remember when supporting an individual with an eating disorder, what would it be?
“Sometimes it is not what people say, but how they say it,” said Dr. Geller. “The way that we speak to our patients, and their experience of how they’re spoken to, is important and has an impact on their motivation, their interest in treatment, their ability to benefit from treatment, and even how much they benefit from treatment.”
“Individuals working on recovery are often struggling even more than before, as they have to find new ways to cope,” she expressed. “It’s very important that care providers recognize their patients’ courage and strengths and also demonstrate that they too practice self-compassion.”
Struggling with an eating disorder?
The first step is to approach your family doctor and let them know what’s happening. From them, you can receive a referral to a secondary eating disorders program, where you will be assessed and can receive treatment and referral to more specialized treatment at St. Paul’s Hospital or BC Children’s Hospital, if needed.
Other resources:
- The Looking Glass Foundation offers a number of great services including Bridge the Gap, which provides affordable one-to-one therapeutic support, and Hand in Hand, which connects you with a volunteer who has similar experiences and interests.
- Jessie’s Legacy provides a wealth of information through factsheets, educational events, and more.
- National Initiative for Eating Disorders has a host of information and resources available, not only for individuals with eating disorders, but also for their family and friends who are looking for support and ways they can help.
This story originally appeared on the CHEOS website.





