Finding a potentially cancerous lump in your breast is traumatic, with both patient and doctor keen to remove it quickly.
But current practices can make the process uncomfortable and stressful.
Now, a procedure using Canadian technology that is in use at Providence Breast Centre at Mount Saint Joseph Hospital is improving the experience for both patients and surgeons. The hospital, the first in BC to use this particular technology involving a magnetic seed (other technologies use radioactive ones), performs about 1200 breast-cancer surgeries each year. That’s more than any other hospital in the province.

Usually, radiologists mark the location of a tumour to be removed by inserting a long metal wire (or wires) into it, says Dr. Amy Bazzarelli, a surgical oncologist at the centre. The patient must then wait at the hospital for surgery, sometimes for hours, while the other pre-operative steps take place. Meanwhile, the wire protrudes from her breast.
But thanks to the technology, funded by St. Paul’s Foundation donors like Doug and Teri Loughran, radiologists can insert a tiny, 3.2-millimetre magnetic “seed,” or marker (about the size of a sesame seed) into the tumour so it can be removed with greater accuracy.

Device adds precision and efficiency, reduces discomfort
After insertion, the patient goes home and returns to normal life until her surgery day.
“She doesn’t have to wait around for the perioperative part as long. It’s a big improvement,” says Dr. Bazzarelli.
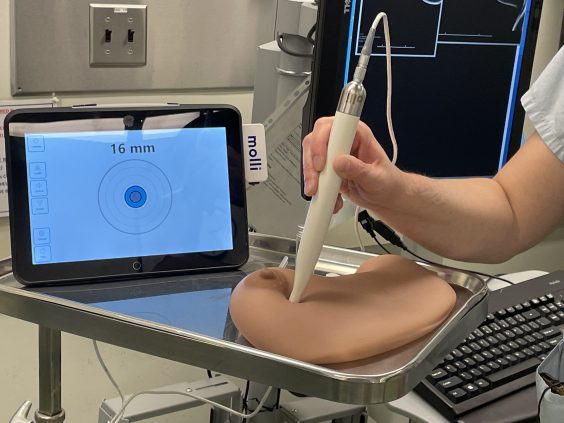
When it’s time to excise the lump, the surgeon rolls a magnetic wand over the breast to locate the seed inside it. A digital tablet connected to the wand emits audio and visual cues for greater precision. As the wand moves closer to the seed, a sound on the tablet gets louder. The tablet indicates the distance from seed to wand.
The wand also detects the seed in the tumour after it’s removed, to confirm it is out of the patient’s breast.
The seed device has added precision and efficiency to the process of breast surgeries while reducing the discomfort, says Dr. Bazzarelli.
The breast-marker technology was developed by a Toronto company, MOLLI Surgical, that is a spinoff from Sunnybrook Health Sciences Centre.
“Traumatizing to see (wires) sticking out of your breast”
Breast-cancer patient Kim Brown is well placed to compare both techniques of tumour removal, one with the wire and one with the breast seed.
She has undergone two breast-cancer surgeries at Mount Saint Joseph. The first was in 2005. Almost two decades later, though, the cancer returned. She had her second surgery last year.
The first time, she required the wires. “I did not like them at all. They’re painful. When you’re waiting, it’s traumatizing to see them sticking out of each side of your breast.”

The second time, the seed was implanted two days before surgery. Brown says it was a vast improvement.
“I didn’t freak out”
“It was painless. I didn’t freak out, whereas you can physically feel the wire. And my recovery time was a lot quicker with the seed. The pain threshold is lower.”
Dr. Bazzarelli says feedback gleaned from questionnaires has been positive for both practitioners and patients.
“This also solves a “flow” problem within surgery,” she says, a term referring to providing patient care smoothly and efficiently so they don’t have to spend too much time in the hospital. “It’s one less step.”
“We hope this becomes our standard of treatment in future.”
Story by Ann Gibbon, Providence Health Care





