Emergency departments (EDs) are critical entry points to the health care system. A research team based at St. Paul’s Hospital is helping shape the future of emergency care in Canada.
For over 30 years, the Emergency Medicine Research Group has been studying how to improve care for patients who come through the ED.
Affiliated with Providence Research, this Clinical Academic Research Group is led by clinician-scientists conducting groundbreaking studies across a wide range of emergency health topics.
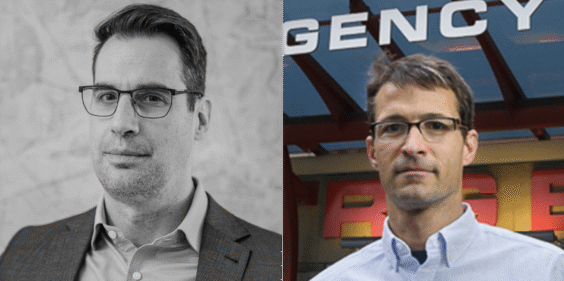
The group was created in 1994 by Drs. Jim Christenson, Grant Innes, and Eric Grafstein to embed research into the fabric of emergency care at St. Paul’s Hospital. Dr. Christenson served as the inaugural Research Director, a role now held by Dr. Frank Scheuermeyer, scientist and program head for emergency medicine with the Centre for Advancing Health Outcomes (Advancing Health).
“It is relatively rare, even in big emergency departments across Canada, to have that kind of focus and culture – that research is not only important, but necessary,” says Dr. Christenson, also an Advancing Health scientist.
Researchers within the group collaborate with each other, and with national research groups, to advance emergency medicine research and improve patient care.
Why emergency medicine research matters

Emergency medicine is a unique branch of health care. While ED physicians are specialized in emergency medicine, they must also be generalists, prepared to manage any condition a patient presents with.
“We need emergency physicians to have a huge amount of knowledge in their brains, to be able to take care of anything that comes through the door,” says Dr. Christenson.
As patient volumes rise, driven by factors including population aging and growth, EDs face increasing pressures. Research provides the information needed to make evidence-based decisions that improve outcomes and efficiency.
“At St. Paul’s, we try to study conditions that are important to our patients, their caregivers, and our staff,” says Dr. Scheuermeyer.
Research has increased ED efficiency, shaped standards of care
Over the years, the St. Paul’s Emergency Medicine Research Group has conducted influential research in many areas that changed practice.
Kidney stone pain: An early significant collaboration with Vancouver General Hospital, the NARC (Nonsteroidal Anti-inflammatory in Renal Colic) Trial, investigated the use of a nonsteroidal anti-inflammatory drug (NSAID), Ketorolac, as an alternative to opioids to treat kidney stone pain. The study found that IV Ketorolac was not only just as effective as IV opioids, but just as fast acting. Now, NSAIDs are the standard first-line treatment for kidney stone pain.
Atrial fibrillation: As a cardiac referral center, the St. Paul’s Hospital ED sees many patients with atrial fibrillation, a common heart arrhythmia. Research led by Dr. Scheuermeyer compared two treatment approaches that were regularly used in Canada: an electrical-first strategy and a chemical-first strategy. The study found that both methods were equally safe and effective, but the electrical-first strategy resulted in earlier patient discharges, helping to free up vital space in the ED more quickly. Dr. Scheuermeyer has also conducted research into identifying high-risk atrial fibrillation patients who cannot be treated with traditional methods.
Substance use and overdose: A major focus of the research group is substance use and addictions. Dr. Andrew Kestler, Advancing Health scientist and St. Paul’s emergency physician, leads research on ED-based interventions for opioid use disorder, integrating research with quality improvement initiatives. One such study demonstrated that overdose patients treated with naloxone could be safely discharged after one hour, instead of the previous standard of twelve, improving efficiency.
The ED is often the last point of contact with the health care system for people who die from overdose. Much of Dr. Kestler’s work surrounds using this opportunity to offer treatment to patients who use substances.
“The whole idea of a lot of the work I’m doing, is using the opportunity of the emergency department encounter – even if they’re there for a sprained ankle, belly pain, or whatever brings somebody in – to use that opportunity to screen for substance use,” says Dr. Kestler. One of his projects showed that enrolling patients in outreach programs directly from the ED increased treatment retention and improved their connection to community care.
Remote Indigenous care: Dr. Christenson is currently leading an initiative to improve emergency care for remote Indigenous communities on Vancouver Island, where access to trained medical personnel is limited. His research aims to identify gaps and advocate for solutions to reduce disparities in care.
Cardiac arrest response: The St. Paul’s Hospital Emergency Research Group has contributed significantly to pre-hospital care with paramedics and Fire Department first responders. Dr. Christenson, with Dr. Brian Grunau, co-directs the BC Resuscitation Research Collaborative, (BC RESURECT), which gathers and utilizes province-wide data on cardiac arrest to improve care and outcomes. Learn more about BC RESURECT here.
Proximity between new hospital, research centre will further connect research and clinical care

As emergency medicine evolves, the St. Paul’s Hospital Emergency Medicine Research Group will continue to develop new knowledge and improve emergency care. The upcoming move to the new St. Paul’s Hospital and adjacent Clinical Support and Research Centre (CSRC) will further integrate research with clinical care. The proximity between the new hospital and CSRC will enhance collaboration between the ED, clinical services within the hospital, and other research groups.
The St. Paul’s Emergency Medicine Research Group’s pioneering work exemplifies how research can directly transform clinical practice, improve patient outcomes, and shape national standards of care in this crucial area of medicine.
“Everyone has either had a health emergency or had a loved one who has experienced such an issue. The emergency department is the one place in the medical system where anyone can attend at any time, without a prebooked appointment. It is the public interface between the community and the health care system,” says Dr. Scheuermeyer.
Story by Grace Jenkins, Providence Research.
A version of this story originally appeared on the Providence Research website.





