In 2020, Ron Pavlakovic received a heart transplant due to his idiopathic dilated cardiomyopathy, a form of heart disease affecting as many as one in 250 people. Dilated cardiomyopathy causes the heart to enlarge and its normally muscular walls to thin and stretch, affecting its capacity to pump blood. Pavlakovic, a real estate professional, was not getting enough oxygen to his system, and was struggling with everyday activities like climbing stairs.
He was in St. Paul’s Hospital, one of 18 health and long-term care sites run by Providence Health Care (PHC), receiving a routine treatment when he got the sudden and exciting news that they had a new heart for him. At 1 a.m. the next morning, Pavlakovic received a heart transplant – but his old one did not go to waste. He donated it to the Bruce McManus Cardiovascular Biobank in the Centre for Heart Lung Innovation (HLI), at Providence Research, PHC’s research engine.
What is a biobank, and why are they important?
Biobanks are collections of biological samples, such as blood, tissue, and DNA, that are donated for research purposes and are often stored with their associated health data. These valuable resources empower scientific discoveries that improve health care, accelerate medical advancements, and help address pressing global health challenges.
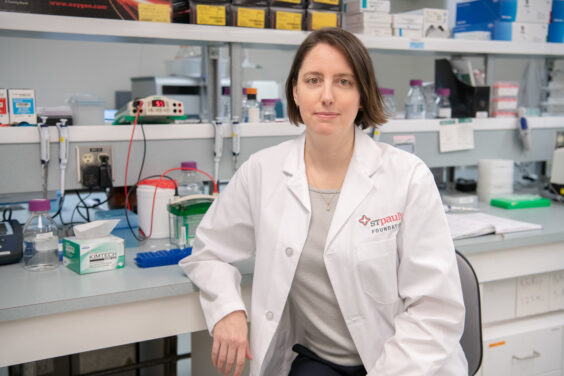
“Creating a biobank is often driven by a clinical need, some clinical demand, some question that remains unsolved in science and medicine,” says Dr. Mari DeMarco, former Research Director of Providence Research and a Clinical Chemist at St. Paul’s Hospital.
Biobanks are essential tools for understanding human health and disease, driving innovation in medicine and improving global health outcomes. They provide a critical scientific resource and means for researchers to access biospecimens donated from patients.
“Biobanks provide invaluable insights into rare diseases and enable the creation of diverse datasets that enhance the inclusivity and accuracy of research, which are key components of precision medicine,” says Dr. Darryl Knight, President, Providence Research, Vice President, Research & Academic Affairs, PHC, and Associate Dean, Research, Faculty of Medicine, UBC. “The importance of biobanks to precision health, information-based medicine, and the quality of health care is becoming increasingly recognized. In addition, biobanking has a huge economic impact, globally valued at around $68 billion in 2021 and anticipated to reach approximately $118 billion by the end of 2031.”
Biobanks drive breakthroughs that can transform how we prevent, diagnose, and treat diseases, ultimately saving lives and improving quality of life for patients worldwide. As part of a unified network, Providence Research provides tools and support for biobank researchers.

Biobanking at Providence Research – our unique focus
Providence Research has a unique focus on biobanking, positioning it at the forefront of research activities. Embedded within St. Paul’s Hospital with direct access to patients, Providence Research is home to a first-in-Canada biobank network collecting a diverse range of samples.
The HLI houses the largest heart and lung tissue biobanks in western Canada, the Bruce McManus Cardiovascular Biobank (BMCB) and the James Hogg Lung Biobank (JHLB). To house these and other specimens, HLI maintains sixty-eight -80°C freezers monitored 24/7 at St. Paul’s Hospital.
“Providence Research has a long-standing history of exceptional biobanking, hosting two world-class biobanks: the Bruce McManus Cardiovascular Biobank and James Hogg Lung Biobank. Over the last forty years, these biobanks have created large and unique biospecimen collections that continue to actively support a growing number of research programs from around the world,” says Dr. Knight.
The JHLB, directed by Dr. Tillie Hackett, contains more than 90,000 specimens from over 3000 patients. Established in 1977 by Drs. James Hogg and Peter Paré, it is the longest-running lung biobank in Canada. It has been a significant resource for lung research, contributing to over 800 published research projects since its founding. The JHLB has been a leader in establishing lung biobanking research protocols that have been adopted internationally, including methods of preservation that allows the samples to be assessed both structurally and at the molecular level.
The BMCB, directed by Dr. Ying Wang, contains over 100,000 human cardiovascular biospecimens with their clinical information, including 544 explanted hearts from heart transplants,14,000 heart valves, and 600 aorta specimens. Established by Dr. Bruce McManus in 1982, it is the longest-running cardiovascular biobank in Canada
Protocols for sample collection can vary, but all biobanks at Providence Research maintain the highest ethical and privacy considerations. When an explanted heart is donated to the BCMB, for example, the patient gives consent to donate their heart for research prior to their transplant, and then later gives specific consent for their sample to be maintained in the biobank. This enables the heart to be retrieved within five minutes post-transplant. It is then taken to the laboratory, where it is anonymized and carefully photographed, measured and weighed before being preserved and assessed by a pathologist, after which it is directed to the biobank for longer-term storage. When a researcher requests the tissue, an appropriate biobank sample is identified, processed, and delivered.
Biobanks advance research through two mechanisms: forward translation, where samples are actively collected for a specific study, and backwards translation, where research is done using pre-existing sample collections. The biobanks at Providence Research provide advice on how to best utilize existing samples and work with researchers to develop tailored collection protocols that best fit their needs. They have an adaptable structure that makes it possible to quickly collect samples for emergent situations such as the COVID-19 pandemic, when biospecimens were urgently needed to understand the virus and develop vaccines and other therapies.
Biobanks at St. Paul’s Hospital uniquely positioned for research
As the home of the province’s adult heart transplant program, St. Paul’s Hospital, run by Providence Health Care (PHC), is uniquely positioned to connect researchers with patients who have the ability to donate critically needed biospecimens, and to bring research directly to patients.
“For almost the entire time that heart transplants have been performed at St. Paul’s, patients have been donating their removed hearts to our tissue bank. This is an incredibly precious and unique resource in the world,” says cardiovascular endocrinologist and HLI Principal Investigator Dr. Gordon Francis, whose research relies on the use of biobanked samples.
The BMCB, located within St. Paul’s Hospital, is one of the few biobanks within Canada that have the capacity for “fresh” biobanking cardiovascular tissue, a process of rapidly freezing tissue after collection that preserves biological integrity and allows researchers to perform a wide variety of analyses.
St. Paul’s Hospital also hosts the B.C. Provincial Renal Pathology laboratory, which receives all diagnostic kidney biopsies in the province. The tissue remaining after the biopsy can be donated to a biobank, and researchers are able to follow up with patients to gather data on their clinical outcomes.
Nephrologist and Centre for Advancing Health Outcomes scientist Dr. Sean Barbour oversees a biobank focused on glomerulonephritis, a term for autoimmune kidney disease, which has a high risk of progressing to kidney failure. Currently, Dr. Barbour is studying the clinical outcomes of anti-nephrin antibodies in focal segmental glomerulosclerosis, to see if these antibodies impact the development and recurrence of the disease. This research could potentially point towards more targeted treatments.
Providence Research is enhancing biobank infrastructure and connectivity
While biobanks have historically operated independently, connecting and sharing resources within and between biobanks can further enhance research and impact. For instance, if two research groups are collecting different types of samples for the same condition, connecting those collections could enable a greater level of discovery than if they had remained separate.
Providence Research is working to enhance connectivity between biobanks within the organization and across B.C. In her role as Research Director, Dr. DeMarco worked to create a modernized infrastructure for biobanks at Providence Research and to ensure that they have the tools needed to be interconnected with the provincial system.
“The vision of Providence Research is to help support provincial infrastructure for biobanking that allows this connectivity between sites, allows the sharing of resources and, where permitted, information,” says Dr. DeMarco. She additionally established a suite of resources to streamline the process of setting up a biobanking program.
Dr. Mei Lin Bissonnette is a renal pathologist at St. Paul’s Hospital and the Director, B.C. Provincial Renal Pathology Laboratory. The laboratory has an archive of the history of renal disease in B.C., which she is expanding into a biobank. She is working with nephrologist Dr. Mark Elliot to create a genetic kidney disease research program as the starting point for this new biobank. Support from PHC and Providence Research, particularly from Dr. DeMarco and her team, has made this undertaking possible.
“This would not be possible without the support of Providence Health Care and Providence Research,” says Dr. Bissonnette. “It’s overwhelming to know where to start, and that’s where the Providence Research Biobank team have been a tremendous resource.”
Dr. Bissonnette aims to eventually expand the biobank and work with other health authorities to offer the ability for patients across the province to donate.
“We are located at St. Paul’s, but we serve every patient with kidney disease in B.C. Whether the patient is in downtown Vancouver or in a more rural area, it’s important that they’re able to participate in research if they’re interested. Their experience can help all of us better understand kidney disease, and how to treat kidney disease in the future,” says Dr. Bissonnette.
Providence Research biobanks advance research into many health conditions
Pavlakovic consented to donate his heart for research. After receiving his heart transplant, he met with BMCB manager Dr. Gurpreet Singhera, who asked if he would allow his heart tissues to be stored in the biobank. He agreed, wanting to contribute to research that could improve care or help develop new treatments for others with his condition. Research from the biobanks at Providence Research has advanced the understanding of multiple health conditions and has identified new targets for treatment and prevention.
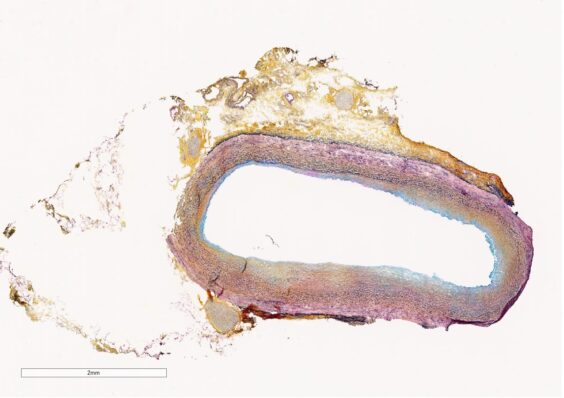
Atherosclerosis, a hardening of the artery wall that is a primary cause of heart attack and stroke, is caused by excess cholesterol being taken up by arterial wall cells. By studying samples from the BMCB, Dr. Gordon Francis determined that most cholesterol accumulates in smooth muscle cells, rather than in immune cells called macrophages, as was previously thought. Having access to arterial heart samples was a major advantage to this research, which could lead to new treatments targeting smooth muscle cells for the reduction of heart attack and stroke.
“We’ve been able to study the basic disease process in the arteries themselves and look at where the disease is happening at the cell level,” says Dr. Francis.
Dr. Stephanie Sellers, an HLI and Centre for Cardiovascular Innovation researcher, leads the Cardiovascular Translational Laboratory, which runs an international multi-centre explanted heart valve biobank. The lab brings together an international network of collaborators to collect a larger variety of heart valves than each individual centre could collect on its own.
“It allows us to get a more comprehensive look at what’s going on in the pathology of these valves, to do studies that allow us to understand how these valves degenerate over time, and to model techniques to replace those valves,” says Dr. Sellers.
While the Sellers lab works at the tissue and cellular levels to understand the process of degeneration, they also run simulations using the explanted valves, including testing them in an artificial beating heart, to better replicate clinical conditions. One recent study demonstrated how calcium deposits on the leaflets of a failed heart valve impact its behaviour when a new valve is inserted.
Cardiologist and HLI Principal Investigator Dr. Zachary Laksman and his team use biobanked heart samples from the BMCB to do genetic, biomarker, and other ‘omics testing. In a recent study, they looked at donated hearts of patients with hypertrophic cardiomyopathy using a new technology called single-cell transcriptomics, which lets them study messenger proteins at a single-cell level.
Where dilated cardiomyopathy, Pavlakovic’s condition, causes the heart’s walls to thin stretch, hypertrophic cardiomyopathy causes the heart’s walls to thicken. Both conditions impact the heart’s ability to pump blood effectively.
By combining this multi-omic approach with clinical testing, advanced imaging, and artificial intelligence, Dr. Laksman’s team seeks to unlock the drivers of disease progression and develop novel therapies for hypertrophic cardiomyopathy.
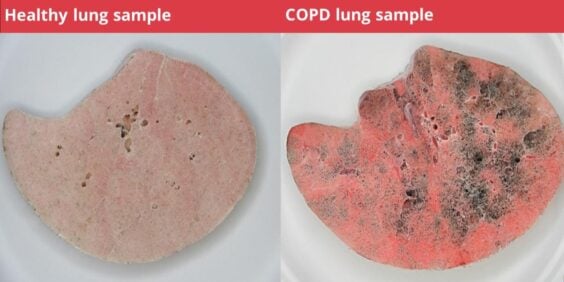
Dr. Tillie Hackett is a Principal Investigator with the HLI and the Director of the JHLB. With samples from the biobank, she and her team conducted a study that found that by the time a patient is diagnosed with mild chronic obstructive pulmonary disease (COPD), more than 40 per cent of the smallest airways in the lung are already destroyed, due to a progressive loss of alveolar attachments that normally hold those airways open. This research is helping shape new guidelines and treatment strategies to diagnose patients with COPD early and prevent lung damage.
These are just a few examples of groundbreaking research enabled by access to the biobanks at Providence Research.
Biobanks play a significant educational role
In addition to research, the biobanks at Providence Research also have a significant educational role. They regularly host tours to help patients better understand their conditions, combat disease misconceptions, and raise awareness about research.
For example, the BMCB and JHLB host tours for high school and UBC undergraduate students focused on dispelling common misconceptions about heart and lung disease, providing the opportunity for students to see the specimens and learn about the importance of biobanks to research.
Donors also welcome to visit the biobanks and have the opportunity during these tours to see their own donated organ. At the BMCB, they can even hold their own heart! Pavlakovic came to tour the biobank at the earliest possible opportunity and found the experience of seeing his own heart fascinating.
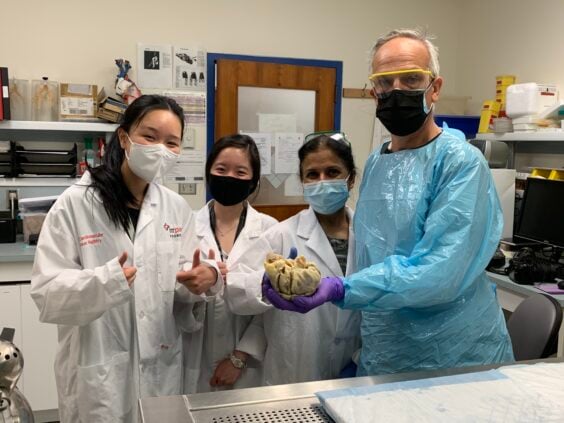
“You get to hold your own heart in your hand. They tell you that your heart is the size of your fist – well, mine was double the size. It had gotten that large,” says Pavlakovic. “You learn a lot, it was eye-opening.”
This experience can often help patients better understand their disease status and risk factors. Pavlakovic had been told by his doctor that his condition was enlarging his heart and causing its walls to become thin to pump properly, but physically seeing it in comparison with a healthy heart sample brought that concept home.
Patients often return years after their tour to thank the biobank staff. Having made a valuable contribution to the advancement of research, they can feel a sense of partnership and closure.
New research complex will have state-of-the-art biobanking facilities
In the Clinical Support and Research Centre, our future research and medical complex, biobanks will be centralized in a purpose-built core facility, designed in consultation with researchers. This highly customized research space will include state-of-the-art collection facilities, specimen processing infrastructure, and dedicated biobank storage space. Bookable drop-down lab space and access to shared equipment will increase Providence’s biobanking capacity and increase accessibility for early-career researchers.
Along with modernizing our research facilities, Providence will be digitizing all biobank collections using OpenSpecimen, an inventory management software that will enable connectivity and enhance visibility of biospecimens. These changes will be reinforced by standardized policies and procedures, creating a first in western Canada, robust and reliable biobanking infrastructure poised to enable groundbreaking research.
The CSRC will be directly connected to the new St. Paul’s Hospital via a skybridge. This proximity will enable researchers to quickly reach patients and give more patients the opportunity to consent to donate specimens to a biobank. The integration of research and clinical care will allow biobanking to be more efficient, reducing the time needed for research to be translated into therapeutic developments.
Biobanking for the future
In the field of medical research, knowledge and technology are constantly evolving, but human biospecimens will always be necessary to advance health research. Biobanks are instrumental in advancing precision medicine – an approach that tailors medical treatment to the individual characteristics of each patient, including their genetic profile.
Supporting biobanks helps ensure that life-saving treatments are accessible and effective for diverse populations, particularly underserved communities, by providing a wealth of genetic diversity in research.
Providence Research’s biobanking infrastructure is capable of adapting as technology advances and new research needs arise.
When biobanks create their sample inventories, they try to keep in mind their potential utility for applications that are currently out of reach. For example, Drs. Bruce McManus and James Hogg both had the foresight to store the samples in their biobanks in ways that preserved cellular structure and RNA, anticipating that more advanced molecular tests would be developed. Now, heart and lung tissue stored decades ago can be used by researchers in ways that could never have been fully predicted from the start.
Biobanks at Providence Research will revolutionize medical research by creating a standardized, globally accessible repository of diverse biological samples and comprehensive clinical data. The implementation of consistent protocols and standardized information will mean that researchers worldwide can confidently compare results and validate findings at unprecedented scales, leading to faster breakthroughs in disease understanding, clinical trials, and patient care.
Bringing the donation cycle full circle
Biobanks are critical in accelerating the development of new treatments, vaccines, and therapies. By providing researchers with diverse biological samples, they help identify new disease biomarkers, uncover risk factors, and evaluate the effectiveness of novel medical interventions.
All biospecimen donations to biobanks, whether they be blood, tissue samples, or whole organs, are vitally important to research that advances patient care. A biobank is most effective when its samples are being actively used in research, not sitting in storage.
“At Providence, we are all stewards of these samples. We want to honour these donations the best way we know how – that is, by getting them into the hands of researchers who can use them to make new discoveries,” says Dr. DeMarco.
All biospecimen donations to biobanks, whether they are blood, tissue samples, or whole organs, are vitally important to research that advances patient care.
“Biobanks are a bridge between scientific inquiry and medical progress. Every sample stored in a biobank holds the promise of a breakthrough, a new understanding of a disease, and a potential solution to a life-threatening condition,” says Dr. Knight.
Particularly for those who donate organs, contributing to a biobank can be a full-circle moment. A person who receives a transplant due to a particular disease or condition, in turn, donates their explanted organ to a biobank, empowering research that could lead to new treatments and preventions for their condition and potentially reducing the need for transplants in the future.
“Donate as much as you can, because they are excess body parts,” says Pavlakovic. “It’s a very thoughtful gesture, and one that doesn’t cost you anything. It potentially gives the people that are studying your condition an opportunity for further research.”
Providence Research biobanks aim to create an enduring legacy that transforms countless lives, enabling researchers to crack the code on rare diseases and helping develop personalized treatments. Our biobanks will break down the barriers that currently slow medical breakthroughs, creating a powerful resource for scientists to access the biospecimens they need to develop a greater understanding of disease mechanisms and leading to better treatments with the potential to turn what are now deadly or debilitating conditions into manageable or curable ones.
For more information on biobanks, contact research@providencehealth.bc.ca
To make a monetary donation to support our biobank program, contact spfoundation@providencehealth.bc.ca
By Grace Jenkins