Bryan Springgay and his wife of 43 years, Laileen Springgay, have travelled the world. Bryan was a Canadian diplomat for over three decades, and every few years the family would get assigned to another post. There were relocation challenges but they embraced the adventures that came with living in different corners of the globe.
But about a decade ago, Bryan, 71, was diagnosed with Alzheimer’s disease/early onset mixed dementia and now lives in a Richmond care facility. The golfer who once hit the links five times a week is still physically strong but his mind and memory are locked. He also has aphasia, or speech impairment. On good days he can communicate a bit with his wife. Most days, Laileen is there to “decode” Bryan’s needs in a way she hopes helps his care providers.
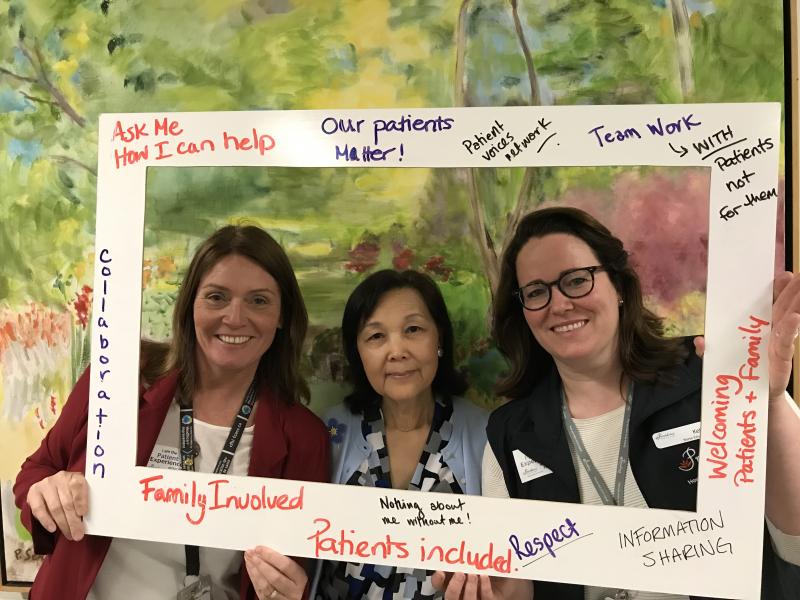
She does so as both a spouse and a patient family partner with Patient Voices Network, a community of patients, families and caregivers working with health care professionals to improve care. She’s part of a committee at PHC that includes practitioners from various disciplines.
This week, she’s involved in Providence Health Care’s Patient Experience Week. She shared her experiences with nurse educators from across PHC to help them forge successful relationships with patients, residents and family members and inspire them to invite Patient Family Partners to collaborate on upcoming education projects.
Laileen was motivated to become a patient/family partner because at times, her experience with the health care system after Bryan’s diagnosis has been challenging. Sometimes she felt her husband’s caregivers weren’t listening to her, despite her repository of valuable information about him that could be helpful. For instance, she was told two years ago he would never walk again. She intervened, got a physiotherapist to work with him and he can still walk.

Bryan Springgay
“There is no one-size-fits-all model of care, especially for the younger, physically active (early onset ) Alzheimer patients. But we are trying to fit them into a hospital model.” She believes families, as health care partners, need to take the initiative and do extra things and share helpful information. “If not, the patient falls through the cracks.”
To describe a successful partnership, Laileen used the analogy of a little lakeside home that a visitor is trying to access. The homeowner is the patient partner and the visitor crossing the lake is the health care provider. There are some jagged edges en route to the house. “You’re great sailors,” she told the educators. “I’m just helping you navigate the jagged parts.”
All this week, the Care Experience Team, headed by Kate McNamee and Kelly Third, are visiting sites at PHC where patients and families can express their appreciation to staff, clinicians, volunteers and patient-and-family partners who made a difference in a loved one’s care.
“It’s been special for me to set aside my typical day-to-day schedule, and venture out to various hospital sites, units and clinics and take a moment to say ‘Thank you’ to everyone who makes a difference for patient, residents and families in our care,” said Kelly. “There are so many great stories from people about why patient- and family- centred care is an important part of their practice.”
Said Kate: “I am privileged to have this opportunity to lead the Care Experience at Providence Health and to stop and spend a few moments during site visits to recognise in person what a difference the people at PHC make in the experience of care for patients, residents and families in clinical, administration and support areas.”