Martin Mannette has been living with chronic obstructive pulmonary disease (COPD) for eight years and he isn’t alone.
An estimated one in 10 people over the age of 40 suffers from COPD – a progressive condition that slowly damages the tissues of the lungs.
Mannette is managing well with a careful combination of medication, but the 68-year-old Vancouver artist is excited about new research that could impact future patients.
A recent study found that permanent lung damage caused by COPD starts much earlier than previously thought, even before patients are showing symptoms. These findings, published July 4 in The Lancet Respiratory Medicine, could dramatically change how patients are treated for COPD, the leading cause of hospital admissions in B.C. and Canada. By 2020, COPD is expected to be the third leading cause of death worldwide.
“I worry about COPD taking over as the number one killer,” said Mannette, “so anything we can do for the next generation so they can avoid COPD is so important.”

Dr. Tillie-Louise Hackett, a Principal Investigator at the Centre for Heart Lung Innovation(HLI) at St. Paul’s Hospital and her research team made the breakthrough discovery. They found that patients diagnosed with mild COPD have already lost a significant portion of their small airways – more than 40 per cent on average.
Currently, patients with mild disease, as determined by a lung function test, are given minimal or no treatment.
“These patients often have little to no symptoms, so it was believed their lungs were relatively undamaged,” said Dr. Hackett, who is also an associate professor in the Faculty of Medicine at UBC. “Now that we know the severity of the damage, we need to look at earlier intervention to ensure the best outcomes for COPD patients.”
The new findings also suggest previous large clinical trials testing new COPD treatments may have failed because patients already had substantial lung damage.
“If the same drugs were tested on patients with more mild forms of the disease, and less tissue damage, the results could be very different,” said Dr. Hackett.
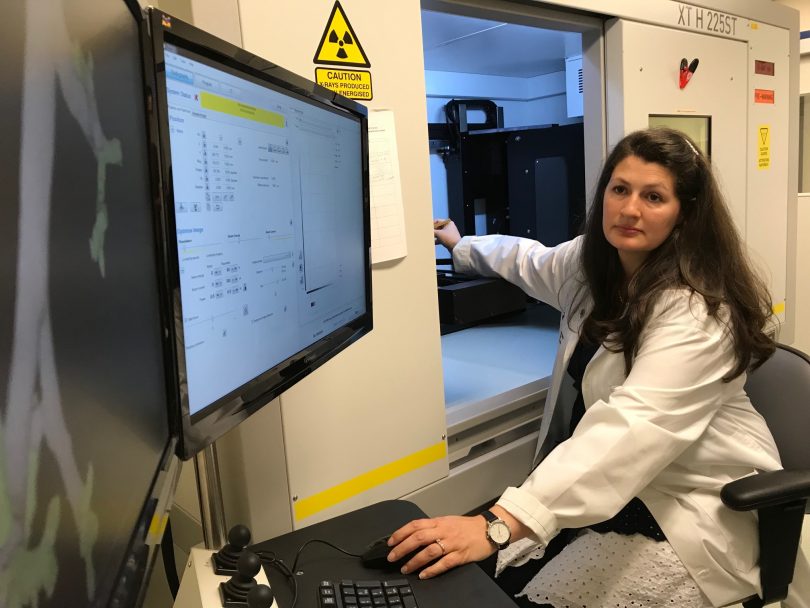
Lung samples from 34 patients were analyzed using an ultra-high resolution microCT scanner, one of only three scanners of this kind in the country. The special scanner, funded by the Canada Foundation for Innovation and St. Paul’s Foundation, was instrumental to Dr. Hackett’s research. Though the HLI Lung Tissue Registry Biobank at St. Paul’s has been collecting specimens for more than 30 years, the recent addition of the microCT scanner made it possible to image samples that are embedded in paraffin in extreme detail.

A lung sample is analyzed with a special scanner.
Dr. Don Sin, Director of the HLI, said the findings have significant implications.
“This breakthrough finding will allow us to develop new drugs to treat patients with COPD at the earliest stages of their disease when the disease is reversible,” said Dr. Sin. “This will prevent disease progression in thousands of patients and help them stay out of the hospital and remain healthy in their own homes.”
Mannette isn’t letting COPD slow him down. He’s currently working on a video project about addiction in the Downtown Eastside and he continues to follow advancements in COPD research and treatment.
“I’m always looking for the ray of light at the end of the tunnel,” he said.