Along with disposable blue gloves, directional arrows in stores and the mantra of physical distancing, the face mask has become a ubiquitous feature of life with COVID-19.
And as the pandemic stretches on, evidence is mounting that masks of all types, whether surgical or cloth, commercial or homemade, plain or adorned with slogans or logos, are effective at protecting us from infection.
St. Paul’s Hospital infectious disease specialist Dr. David Harris was part of an international research team behind a June 1 Lancet analysis of 172 existing studies. The researchers looked into current health measures such as physical distancing, eye protection and face masks, “suggest that wearing face masks protects people (both health-care workers and the general public) against infection …” while cautioning no single measure provided complete protection.
More businesses insist on mask use

The use of face masks is becoming more prevalent as economic restrictions ease. Many shops, personal-care providers and even airlines are making them mandatory. British Columbia is poised to enter Phase 3 of its re-openings and has given the OK to expand “bubbles” of social contacts. All of this means people will be interacting with others in greater numbers.
As the knowledge around the pandemic evolves, there is stronger consensus that if you can’t stay at least two metres apart from others, face coverings should be worn to prevent the virus’s spread.
Mask wearing protects others
As Dr. Don Sin of Providence Health Care’s Centre for Heart Lung Innovation explains, COVID-19 is transmitted to others via droplets (or “micro spit” as he describes them) from the mouth. “The masks trap the droplets so the virus cannot be transmitted to others if we are carrying it in our nose or mouth.”
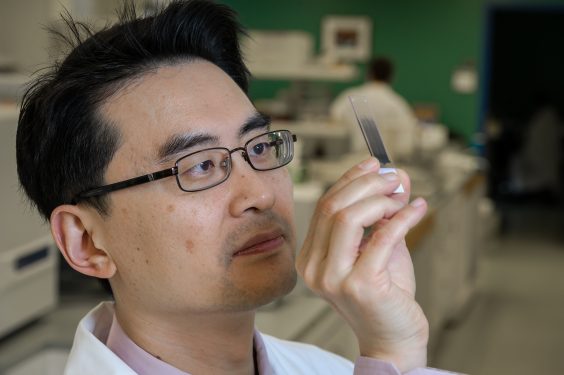
A strong proponent of masks, Dr. Sin says, “I’m a believer in wearing one all the time outside of the home. There is little downside.”
Aggie Black, Director, Health Services & Clinical Research and Knowledge Translation in PHC’s Professional Practice Office, says the main principle of mask-wearing is that it protect others. “You can be asymptomatic and be infected. You can have a false negative. If I don’t know I have it and I don’t wear a mask, it’s putting others at risk.”
As mask wearing becomes more prevalent, so too do questions around their use. Dr. Sin and Black weigh in on some of common questions:
1. Should everyone wear a mask?
While health officials say most people should wear masks if physical distancing isn’t possible (and health-care workers must wear surgical masks), Black says they could pose a challenge for some, like people with cognitive impairments such as dementia. Dr. Sin says those with severe chronic obstructive pulmonary disorder (COPD) or severe heart failure “may feel claustrophobic wearing a mask.” The BC Centre for Disease Control says infants under two should not wear face masks or coverings because their airways are still small and they could have breathing difficulties. While there have been anecdotal reports of people with good health reporting breathing difficulties, Dr. Sin says with proper masking techniques, people won’t develop breathing issues.
2. What are those proper techniques?
Dr. Sin advises the following steps:
- Wash your hands before touching the mask;
- Touch the mask by its strap or ear loops;
- Carefully place the mask over the face, ensuring that both nose and mouth are fully covered;
- Place your fingertips from both hands at the top of mask to mould the nose area to the shape of your nose, and;
- Check that there is no air leak around the mask.

3. What about when you’re jogging outside, or hiking?
Dr. Sin allows that the risk of contracting COVID-19 outdoors while exercising outside is low, and masks may not be needed. “But personally, I would wear a mask while hiking or outdoors in general unless I’m really uncomfortable. The risk is lower outdoors for sure, but it is not zero.”
4. What is the best kind of mask?
Dr. Sin says the best masks are medical N95s, but they are expensive and less-well tolerated. They should be reserved for health-care workers. They must also be properly fitted. Surgical masks with good seals around the mouth are acceptable for most people. Cloth masks should have multiple layers of fabric to increase their filtering ability, which can reduce transmission. Cloth masks can be made from commonly available materials like sheets of tightly woven cotton. (For more information on masks visit the BCCDC here).
5. How often should people replace their masks?
It depends on whether you’re a health-care worker or not. Aggie Black says that after a period of time, “We tell staff that the outside of your (surgical) mask is contaminated with other people’s droplets, which may include COVID-19.” For that reason they are advised to remove their mask and dispose of it, then clean their hands and wear a new one. “If you’re in a non-health-care setting, you could probably re-use masks.” Cloth masks are reusable but must be washed regularly, according to the BC CDC.
6. Any final thoughts?
Both experts agree: Jurisdictions where mask wearing was common pre-COVID have fared well in the crisis. Black notes: “Countries with a mask culture are doing better.” Dr. Sin says: “Japan has almost completely suppressed COVID-19 through good hand hygiene and mask use. Tokyo is so dense that social distancing is difficult but it was able to control the disease by widespread use of masks.”





