Sound returned to Alan Holt’s world in late 2017 when surgeons at St. Paul’s Hospital inserted a cochlear implant (CI) into his right ear. Music, bird song and the laughter of his grandchildren returned to his life after years of diminished hearing, caused by a career in a noisy Sunshine Coast pulp and paper mill. Things eventually deteriorated to the point where hearing aids he used were no longer effective.
Each year since receiving the implant, the 68-year-old retiree has returned to St. Paul’s for a follow-up that involves reprogramming the device, a process called mapping. There, a CI audiologist programs and adjusts the external sound processor to his specific hearing needs.
Holt, a resident of Duncan on Vancouver Island, is grateful for regaining his hearing, especially after two near accidents with vehicles driving behind him as he walked on a rural road (without sidewalks). He could not hear them.
“It was a life-changing surgery,” he says.
As thankful as he is, Holt must carve out a full day for his follow-ups, because St. Paul’s is the sole provider of cochlear implant services for adult residents of British Columbia and Yukon through its BC Adult Cochlear Implant Program.
For two years, the follow-up day went like this: Holt rose at 4.30 am to drive to Nanaimo for the 8.15 am ferry, then once on the mainland, drove to the hospital for his 90-minute appointment. He grabbed a meal then drove to the ferry for the 5.30 pm sailing, returning home at 9 pm, exhausted.
Travelling to and from the clinic “a real hassle”
“It’s a long day,” says Holt. “The whole experience of driving in the city, trying to find parking – it adds a whole bunch of stress. It’s a real hassle and it takes a lot of time.”
He was dreading this year’s appointment in particular because of COVID-19 risks around ferry travel.
A first for BC adults
As it turns out, the 2020 visit to the clinic has been dramatically different. And Holt is thrilled about it.
St. Paul’s has partnered with Island Health and Provincial Health Services Authority (PHSA) to set up the first remote adult-mapping program in BC. It launched December 4. The plan is for patients to have their annual follow-up visits through telehealth though they’ll be seen in-person every three years for physical check-ups.
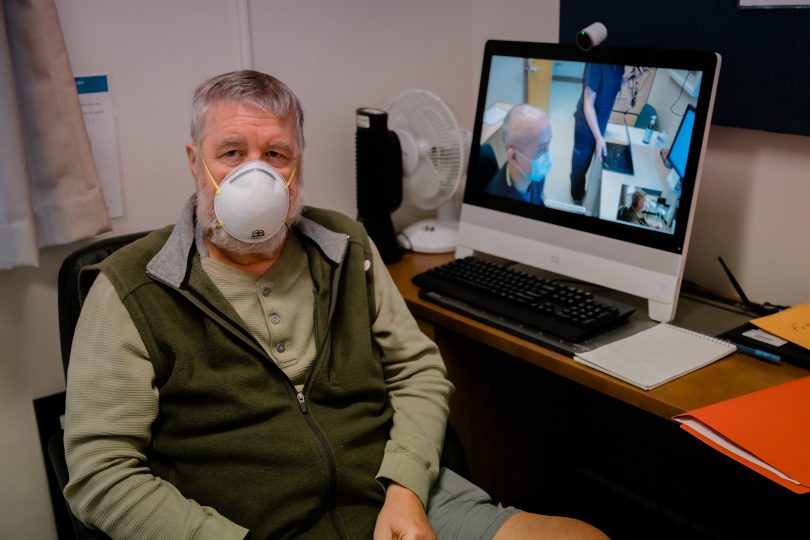
Holt is one of the first virtual mapping patients. On this December day, St. Paul’s CI audiologist Myron Huen uses a sophisticated video platform to remotely test Holt’s processor, far from where he sits in a clinic at Victoria’s Royal Jubilee Hospital.

“How’s the hearing?” Huen asks Holt, whose image looms large on her monitor. “Your battery is good and tight? We’re going to remap to make sure your hearing is as optimal as it can be.”
The two communicate with each other via computer screens, and Huen spends the next 90 minutes painstakingly fine-tuning Holt’s device. When she has to deactivate the implant, she types what she’s doing on a screen Holt can see on his screen. She will test an array of 22 electrodes implanted inside Holt’s cochlea, the snail-shaped part of the inner ear that lets people hear. (Cochlear implants work by bypassing damaged portions of the inner ear and then directly stimulating the auditory nerve leading to the brain. They involve internal and external components).
COVID-19 expedited the virtual program
Virtual health has become a hallmark of many aspects of patient care since the pandemic, and this clinic is no exception. “This program has been years in the making, but COVID gave it a real push,” says Huen. “With COVID, telehealth has been a central part of health-care delivery.”
“Caring for patients virtually is part of our long-term digital strategy at Providence,” says Brian Simmers, the organization’s Chief Financial Officer.
“Creating partnerships like this remote mapping cochlear implant program provides seamless care for our patients. Technology like this enables patients to receive care closer to their homes, while connecting virtually makes it a smooth experience for both patient and health care provider.”
CI audiologist Jowan Lee, who treats CI patients virtually and in person too, gives the program high praise. “It’s so seamless, it’s like the patient is right in the room,” he says. “This remote mapping service was made possible because of the collaboration with virtual-care services at Island Health and Providence, and the IT wunderkinds at PHSA and Island Health. They did the meat of the work and I’m the one who benefits, along with the patients.”
Dr. Mary Lyn Fyfe, Island Health’s Chief Medical Information Officer, says: “We are profoundly impressed by the collaboration among our interdisciplinary team members in creating this virtual inter-health authority service. Each individual understood the significance of this program, especially during the pandemic, made it a priority and, thus, a reality for our Island residents.”
Goal is to expand remote mapping clinics
Vancouver Island was chosen because of the high number of people with cochlear implants, about 180 patients. Lee says the goal is to possibly expand the virtual clinics up the island then, if things go smoothly, to Interior and Northern Health. “People there have insanely long days to get to the clinic – often a 10-hour drive, depending on where they live.”
The virtual clinic can potentially ease the burden from the in-person clinic, where space is at a premium, and in so doing, allow audiologists to see more patients in person.
Alan Holt is more than happy with his first virtual appointment. “It was a really good process. There was no waiting at ferry terminals, no trying to find parking in downtown Vancouver or getting up early.” He was home by 1.15 pm – a good eight hours earlier than usual. “It was a huge savings in time, cost and stress reduction.”