Mother’s Day is traditionally a time to celebrate the women who nurture and care for us: our mothers, grandmothers, stepmothers, aunts and other people who fill those roles in our lives. We honour their love, loyalty, and dedication to their families. But lost in all the celebrations is the darker, more challenging side of motherhood that can emerge during pregnancy or with a newborn.
Transition to parenthood is huge and challenging
“So often, we place so much emphasis on the right crib, the right stroller, or the right swaddle,” says Michelle Carter, clinical nurse specialist in psychiatry at St. Paul’s Hospital. “We don’t focus enough on the transition; the adjustments a new mom has to make to her lifestyle and her relationships. This transition to parenthood is huge and inherently challenging.”
When it’s more than the “baby blues”
The vast majority of new moms (approximately 80 per cent) will experience what is known as the “baby blues”. This low mood, which can have new mothers feeling incredibly sad and tearful, typically occurs in the first two weeks after the baby is born and is a response to physiological and hormonal changes happening in the body. If it extends beyond that time period, and starts to impact a woman’s ability to function, she might be experiencing a perinatal mood and anxiety disorder like postpartum depression and should see her health-care provider.
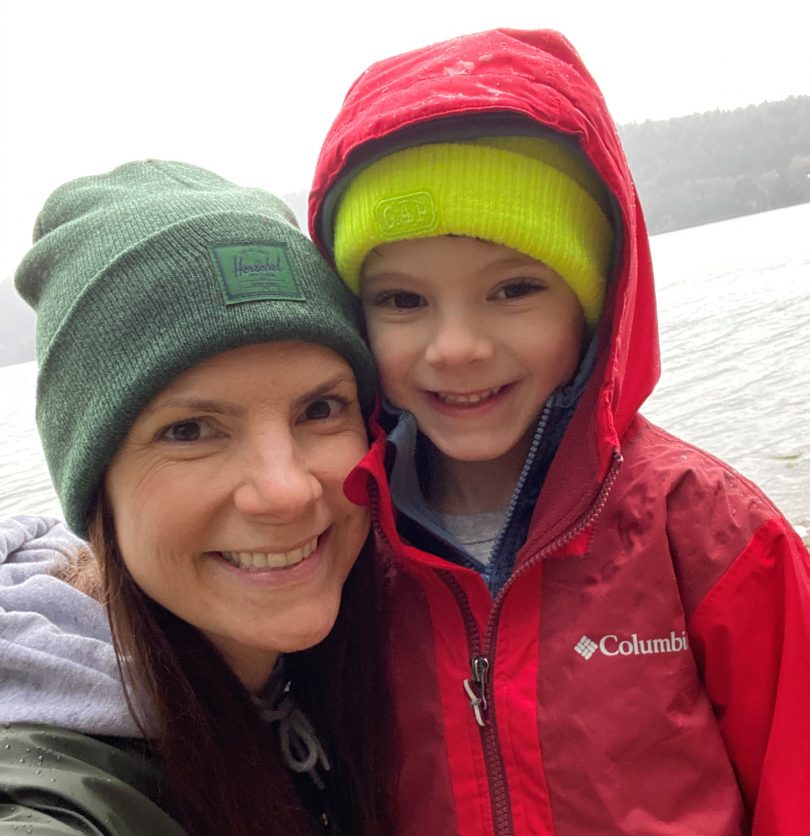
“I had two friends who had babies around the same time as me,” recalls Holly Conway, who gave birth to her first son at St. Paul’s in 2015. “We would call each other and visit with our babies. They were so excited about being mothers. I wanted to enjoy this time with my son, do all the new mom things, but I just couldn’t. I felt like I was faking it all the time. All I really wanted was for my son to grow up and get bigger so I could go back to feeling like myself again,” says Conway, a Vancouver Virgin Radio show host.

It took Conway nearly 10 months to admit she needed some help. “I went to see my family doctor and they told me I was experiencing postpartum depression and referred me to counselling.”
You’re not alone
That referral led her to the outpatient reproductive mental health clinic at St. Paul’s Hospital and Conway credits that team and her clinical counsellor with helping her through this really difficult period in her life.
“I was really unprepared to feel the feelings I was feeling. I had only heard term “baby blues” and knew that should have only lasted a few days,” she says. “I didn’t know anyone who had postpartum depression. I felt very alone, and I thought I was a bad mom.”
“The reproductive mental health team at St. Paul’s is really dialed in to what is going on for women around birth and postpartum,” says Jenna Baumgartner, clinical nurse educator for complex care coordination at St. Paul’s. “They know this part of a woman’s life inside and out. You don’t have to explain what’s going on, they just get it, and you can work with them immediately.”
As Conway did more and more research, she learned that postpartum depression affects up to 20 per cent of new moms. It helped normalize how she was feeling and made her feel less alone. She also learned about the many resources available to support new moms, from public health nurse visits and new mom groups at the community centre to helpful websites.
“I wish I had spoken up earlier. I guess my pride held me back. My husband and family were so supportive when I did finally tell them; there was no judgment at all,” says Conway. “Even with their support, it was around my son’s first birthday before I started to feel like myself again.”
Getting the help you need
“Perinatal mood and anxiety disorders are very treatable. While seeking help can be challenging and vulnerable, it is important,” says Carter, “Untreated disorders also have their consequences and can affect the baby, the mom and their ability to bond.”
The St. Paul’s outpatient reproductive mental health clinic provides diagnosis, therapy and medication, if necessary, for patients who are able to be at home with their baby or family. Since the pandemic, the clinic has moved to offering virtual care, something the team has come to realize actually improves accessibility for new parents who might struggle to attend an in-person appointment while juggling a baby’s feeding and napping schedule.
The mental health and maternity teams also work closely to coordinate care for people with pre-existing mental or psychiatric illnesses who are also pregnant.
Mothering the mothers
“I didn’t talk about my postpartum depression for a long time. I was a bit embarrassed by it,” says Conway. “Now, I make a point of checking in with my friends and my sisters’ friends who are having babies. I want them to know that it is ok to feel the way they are feeling and that they are not alone.”
“It’s so important for new moms to know that it’s ok to ask for help,” says Carter. “You are not alone, you are not to blame, and with help, you will be well.”

Resources for people experiencing perinatal mood and anxiety disorders:
Pacific PostPartum Society
Phone/text support: 604-255-7999
Postpartum Support International
Helpline: 1-800-944-4773
BC Crisis Centre
Helpline: 310-6789