As Larry Schofield heals more each day, he reflects on the vast improvement in his quality of life since his complete ankle-replacement surgery in 2020. “I was…not just recovering from the surgery, but improving far beyond where I was before the procedure.”
Back then, completely replacing an ankle was experimental. However, due to advances in research, it has since become a standard procedure.
CHÉOS Scientist Dr. Alastair Younger, a world-renowned orthopedic surgeon, operated on him. He has been pioneering orthopedic practice and bone-healing research for several years.
He practises out of the Footbridge Clinic in Vancouver and operates and covers trauma on call at St. Paul’s Hospital. Footbridge houses cutting-edge technology for both practice and research purposes. For example, it has one of the few weight-bearing CT scanners that exist in Canada.
Image of the weight-bearing CT scanner at Footbridge Clinic.
“The weight-bearing CT is able to show us how the bones line up when a patient is standing,” says Dr. Younger. That information “gives us a better idea of how the injury or disease is impacting the patient before surgery and how it’s healing afterward when the foot is being used. It is even possible to calculate the percentage of bone healing using a CT scan.”
Imaging inside the foot is useful in clinical research, especially when investigating the impact of different medical devices and techniques used in orthopedic surgery. Dr. Younger has been involved in several clinical trials evaluating how various total ankle-replacement systems, bone screws, operation navigation systems, and surgical techniques impact patient foot repair and healing.
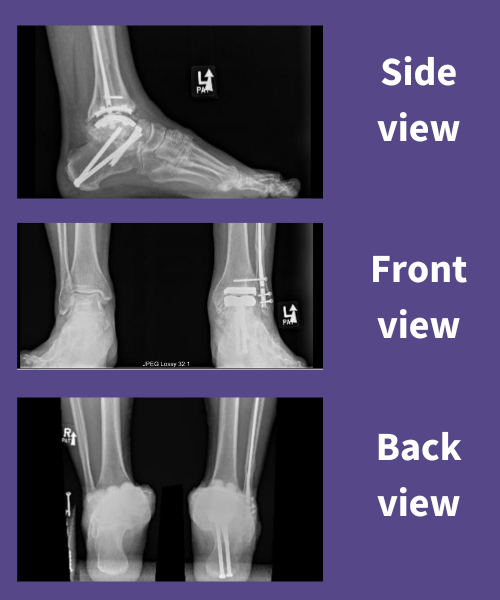
For instance, prior to his full ankle replacement, Larry was involved in two clinical trials evaluating two different orthopedic devices — a total ankle system and a bone screw. “I participated in a study where they were looking at new types of bone screws used to help fuse a joint in the foot together.” He didn’t know if he was getting the newer screw being tested, or the standard screw, but saw a benefit in participating.
Although there are now several devices to support patients’ mobility, Dr. Younger points out that there is a significant gap in understanding how human bones heal. With the advancement of regenerative medicine, there is a possibility to further improve patient outcomes.
Bone healing is universal
“Bones in the foot heal the same way as other bones. When we better understand how they heal, there is incredible potential for improved care,” emphasizes Dr. Younger. “The knowledge gained from learning how bones in the foot heal can be applied to bones throughout the rest of the body.”

While fractures are common and costly, studying fracture healing is difficult. Often, a broken bone is the result of a sudden traumatic event, ranging from sporting injuries to car accidents and causing considerable stress and pain and sending patients to the Emergency Department or Urgent Care. There, the priority is visualizing the bone to determine the extent of damage and then using those images to inform care. The nature of fractures varies a lot, even in fractures of the same bone, and the short timeline in treatment makes obtaining consent from patients to study how their bone heals challenging.
In contrast, reconstructive (fusion and replacement) orthopedic surgery is on a different timeline. Appointments are made well in advance, giving enough time for clinicians, researchers, and patients to discuss participating in a research project or clinical trial. Another significant benefit of studying bone healing in non-urgent, orthopedic-surgery settings is that patient follow-ups are done with the same doctor.
Patients can participate in long-term research
This consistency is not only beneficial for the post-operative care of the patient. It also provides an excellent opportunity for patients and their surgeons to build a relationship. That lends itself to working together on long-term research studies. For example, a recently published study, led by Dr. Younger, showed that less invasive arthroscopic ankle surgery had a lower infection rate than standard open-ankle surgery. Being able to participate in this study involved seeing patients annually for at least five years. In fact, Dr. Younger has been following some study participants for over 15 years.
“Another benefit to studying bone healing in foot surgery is that the bone is quiet and calm until the operation. It would be possible to look at growth factors in healthy human bone and compare them to healing human bone to understand the differences and develop treatments to improve bone healing all over the body,” says Dr. Younger.
Not only would investment in bone healing research would be undoubtedly applicable to aiding the recovery of broken bones throughout the body, it would also help in understanding why and how hip and knee replacements fail, an issue that is strongly related to poor bone healing.
Taking a long time to ‘kind of’ heal
Bones break, and they break often. In fact, in 2019 there were 178 million new recorded bone fractures internationally, with an additional 455 million recorded cases of patients experiencing symptoms from bone fractures dating back nearly 30 years earlier.
Larry’s foot injury is the perfect example. While it happened in his late teens, he never quite recovered.
“I broke my ankle playing sports and underwent surgery. The talus bone in my foot had to be screwed together. It healed quickly after surgery, but then the joint wore very early and quickly because I was very active and continued playing soccer and running 5–10 km a day.” About 20 years later, he had to have another surgery, called a debridement procedure, to help clear some of the debris that had built up over the years, causing pain and clicking noises in his ankle.
An earlier surgery yielded terrible results
Larry’s foot did not heal well after the debridement procedure: “I did not walk for a year; it was a catastrophic failure.” He figured it may have been his body reacting to the procedure, which had resulted in a great deal of post-operative scar tissue that eventually made his range of motion essentially zero.
That was when Larry knew he needed to find another solution. He was referred to Dr. Younger for complete ankle-replacement surgery. At this point, over 40 years had passed since the initial talus bone fracture, and in that time, ankle debridement procedures had been removed from surgical practice due to the high failure rate.
Running again after two decades
From living in chronic pain with limited mobility to exercising daily on local trails and in the gym, Larry is able to fully experience and appreciate moving again.
“I can run again, which I haven’t done for 20 years,” he says. “I’ve lost nearly 50 pounds and can confidently say that the ankle replacement surgery was life-saving. I’m happier to be living a far healthier lifestyle now and am enjoying every minute of it.”
Both the frequency of bone fractures and how long they disrupt patients’ quality of life means that orthopedic care is in high demand. In fact, prior to the opening of the Footbridge clinic in 2018, patients had to wait upwards of six years for just a consult. Now it takes between four to six weeks.
Biobanking potential
With nearly 80 per cent of consults leading to surgery, there is plenty of opportunity to do research on healing bone, especially in collaboration with the growing biotechnology industry. Dr. Younger is interested in biobanking to store tissue from surgeries and investigate healing processes, as well as engaging in machine learning to help understand variables that may positively or negatively impact healing after surgery.
When asked if he would donate un-needed tissue to bone healing research, Larry says absolutely. “If my contribution can prevent at least one person from going through the same pain that I did, I would gladly help”
By Alison Müller, Centre for Health Evaluation and Outcomes Science. This story is adapted from the original version, here.





