When Angela Steininger learned she needed a life-sustaining cardiac procedure, her first thought wasn’t about having the treatment. Rather, it was how she could schedule her medical appointments around her active lifestyle. “I said, ‘Can we have our call before 10:30? That way I can still ski at 10:30,’” Steininger recalls with a laugh.
Her priorities might have raised eyebrows on her health care team, but they wouldn’t surprise anyone who has spent even five minutes with Steininger. As a grandmother of four and an avid sailor, kayaker, and skier, Steininger puts caring for her loved ones and spending time outdoors at the top of her priority list.
But as her procedure approached, Steininger was busier than ever. “I really wasn’t focusing too much on myself,” she says.
Care plans for patient lifestyles
That’s where the nurses at St. Paul’s Hospital stepped in — not only to put Steininger first, but to create a compassionate care plan that meshed with her lifestyle. They provided over-the-phone advice when she couldn’t come to the hospital and they kept her spirits high during tense moments.
“I received such personalized service. I felt that I was someone of genuine significance,” says Steininger.
Steininger’s story is part of a long line of remarkable experiences between patients and nurses at St. Paul’s. Indeed, it’s fair to say that the hospital’s 130-year tradition of nursing leadership continues to attract the best and brightest to its halls.
“Nurses occupy that incredibly vulnerable space between the stretcher and the curtain: in the clinic, in the emergency department, even on the streets,” says Dr. Sandra Lauck, who is both an RN and a PhD. “No one spends more hours with patients and clients than nurses.”
Now, in a bold move to leverage the expertise of its nurses, Providence Health Care is creating CREST: the Centre for Research Training for nurses and allied health professionals. CREST is an exciting initiative that will provide training, infrastructure, and funding to support and encourage staff as they advance their clinical and research careers.
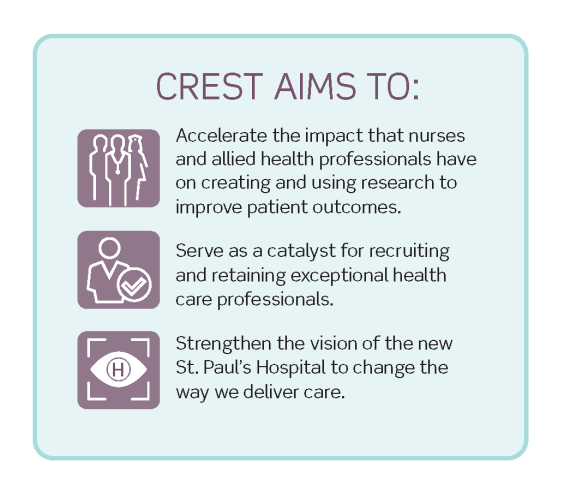
Not only will CREST help ambitious nursing and allied health scholars to excel, it promises to narrow the gap from the researcher’s bench to the patient’s bedside.
Mining the potential of clinician-scientists with CREST
As a clinical nurse specialist at St. Paul’s, Michelle Carter is already engaged in research to improve patient outcomes. Carter is using her in-hospital experience and her master’s degree to improve systems related to reproductive psychiatry.
“I facilitate cognitive behavioural therapy groups with perinatal patients. I help develop new programs for our clinical teams, for example, setting up virtual outpatient clinics during the pandemic. And I collaborate with researchers on a variety of studies,” she explains. “No two days are the same, and that’s part of why I like it.”
Because Carter interacts directly with patients, her work is already bringing valuable patient experiences into her research (which is often done outside of the hospital environment).
Speech-language pathologist Kate Davies says this is the same gap she hopes to bridge. Her research centres on analyzing dementia-related impairments to identify patients’ communication challenges and develop solutions.
“A lot of health care research, especially in the early stages of the study, is done by people who may not have direct – or recent – clinical experience,” Davies explains. “So a lot of the treatments they’re working on, while interesting and promising, are extremely difficult for clinicians to actually implement with patients.”
She hopes CREST will support researchers like her who want to improve patient outcomes and health system effectiveness. “CREST will create an environment between a university and a hospital. In other words, a bridge between research and care,” she says.
“CREST won’t just encourage new research, it’s going to encourage creative, ambitious clinician-scientists to come into the field.”– Michelle Carter
Filling the “missing middle”
Davies and Carter are among hundreds of nurses and allied health professionals who have undertaken research to improve care for patients, long-term care residents, and families at Providence over the last decade.
Of course, research takes time, training, and support. Lauck is confident CREST will provide the resources and unique mentorship for researchers like Davies and Carter to thrive and to remain engaged in the profession.
“This is a really sensitive issue right now because we’re facing a nursing shortage,” says Lauck. “But part of the reason nurses are leaving the profession is because opportunities for professional development, particularly in research, are not always available.” This is what Lauck refers to as the “missing middle.” That is, master’s, PhD, and post-doctoral level professionals who want to further their careers as research-intensive clinicians, but who don’t currently see a path forward.
With mentorship, collaboration, and support with other research essentials (things like grant writing and teaching), CREST will keep talented professionals engaged and anchored not just at Providence, but within the health care system.
As Lauck says, “We are not trying to take people away from the bedside. We’re trying to create opportunities to bring more people to the bedside.”
Home is where the science is
As for Steininger, after her stay at St. Paul’s, she has a renewed appreciation for the unique and irreplaceable role of nurses. And she’s now on a mission to give back as a patient partner in nurse-led research.
“Nurses as researchers make so much sense,” says Steininger. “There are so many things that only nurses do and that only nurses will notice.”
With the advent of CREST and the support of patient partners like Steininger, Lauck sees a very bright future for passionate nursing and allied health researchers – and for patients across British Columbia.
This story by Leah Bjornson was first published in the 2023 edition of Promise Magazine.





