A year ago today, health care as we know it was upended.
On March 11, 2020, the explosive rise of COVID-19 cases prompted the World Health Organization to declare a pandemic. Strict measures were imposed everywhere, including in BC hospitals and care homes, in order to stave off rising infections and deaths and keep staff and patients safe.
Providence Health Care, like so many health-care organizations, was front and centre in the crisis, under intense pressure to keep patients, residents and staff safe, while working with Vancouver Coastal Health and other health partners to brace for a potential surge that could overwhelm the health care system.
In the past year, filled with enormous pressure, human suffering and loss of life, the people at Providence have shown resilience, ingenuity and an ability to turn on a dime to adapt everything from walk-in clinics to lab-testing capacity in the face of the deadly virus.
PHC has retooled some projects, ramped up others and begun new COVID-specific work altogether.
Read a few of the many ways PHC has come together in the past year for a common purpose: adapting to the deadliest, most demanding health crisis in over a century.
St. Paul’s Hospital establishes a COVID unit
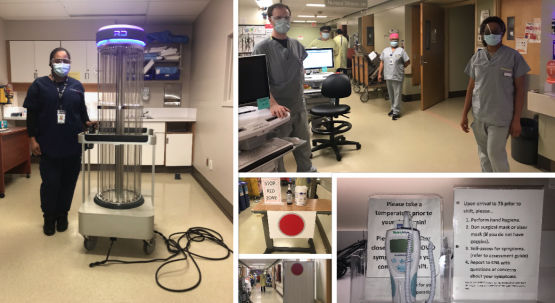
This was an early change. Last year, the 7B unit at St. Paul’s Hospital – previously a Medicine Unit serving patients with a range of illnesses – was chosen as the preferred location to care for COVID-19 patients not in need of critical care.
The layout of the unit allows for complete and total separation between the red zone, where teams care for COVID positive patients, and the yellow zone, where moderate-to-high risk patients await their swab results.
The colour-coded system divides all units of the hospital into green, yellow or red zones, indicating the presence of COVID-positive patients in the area and the subsequent appropriate level of PPE and other precautionary measures required in that area.
The nurses in the red zone are physically separate from the nurses in the yellow zone. Each zone has its own break room, staff bathroom and secure drug storage unit. Signage on the unit indicates the boundaries of the red zone, which adjust regularly as patient numbers ebb and flow.
Teamwork is everything on 7B. An LPN or patient-care aide runner in the yellow zone helps reduce the risk of transmission by supporting the nurses in the red zone to access supplies. The housekeepers, who are the backbone of the unit, service the area with enhanced cleaning protocols. The vast majority of the team have been working on 7B since the first COVID patient arrived on the unit. As patient numbers have increased, so has the size of the team and its level of expertise.
Screeners at entrances ensure visitor safety

Patient and staff safety of course became paramount at sites once the WHO declared pandemic. Pre-pandemic, visitors to a Providence site came and went freely. Today, they meet screeners at the entrance who ask COVID-related questions to ensure everyone’s safety, offering a medical mask if needed and providing hand sanitizer. Screeners have the drill down to an art now and visitors know what to expect.
In the early days of the pandemic, almost 100 people stepped up to volunteer, helping when and where the need was most urgent. The biggest challenge for the greeters and screeners in the pandemic’s early days was how to keep track of the ever-changing visiting requirements. Now the role has become a full-time position, a nod to its critical importance.
PHC sets up COVID-19 testing centre

The St. Vincent’s COVID-19 Assessment Centre at Heather and 33rd Avenue, was transformed from an unsuspecting parking lot almost over night.
That speed belies the hard work that went into creating the site on a tight deadline, says Anthony Munster, Executive Director of Providence Projects, Planning & Facilities Management. As well, strong team work continues to keep the site going, serving the approximately 250-400 people that show up daily for tests. (The record was 500 people tested in under eight hours.)
At the heart of the successful site is a unique collaboration. Vancouver Coastal Health runs the clinical operations, while Providence supports the every-day operations, including registering each visit into the system and operating security, ongoing maintenance of the facilities and daily deliveries of supplies.
The site team has proven their adaptability and resilience over the course of the four seasons. One of the highlights was when it seamlessly switched out the wedding tents – they served well during the first spring months – for the heavy-duty winterized tents currently, all without missing a single test.
PHC Lab is reconfigured to handle COVID tests
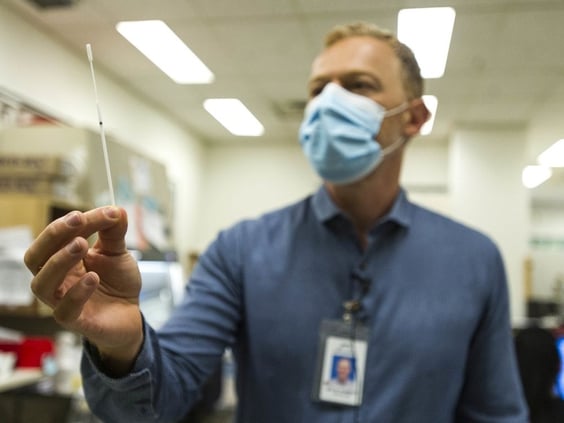
Last year, when it became clear that testing had to ramp up for an emerging mystery virus from Asia, the St. Paul’s Hospital Microbiology and Virology Lab got creative.
By February 2020, the team created a contained space to test in a way that was safe for lab staff. Within a day, a lab wash-up room became a COVID-19 molecular extraction room. Then temporary walls went up around highly automated viral-load instruments. The space was configured into a negative pressure area so air would flow from inside the lab to the outdoors, avoiding other parts of the hospital.
In January 2020, the team bought and refurbished a used molecular-extraction instrument from a Boston lab, originally to increase non-COVID virus testing. When it arrived in March, its role quickly changed to test solely for COVID-19.
Other changes included expanding hours to deal with the increased testing volume and adding staff.
Earlier this year the lab started testing for COVID-19 variants.
Ambulatory clinics go virtual

As a provincial leader in the delivery of number of specialty health care services, Providence is no stranger to virtual health care. Telehealth has long been a part of the care model for patients who live outside the Lower Mainland to supplement and reduce the frequency of travel and in-person appointments.
But when the pandemic struck, moving care to a virtual space was no longer just a matter of convenience – virtual care became essential to ensure the safe continuity of care for patients, wherever they were.
Across the organization, teams quickly adapted a number of important patient programs so they could be delivered virtually: prenatal classes, Eating Disorders support services, and the first remote Cochlear Implant adult-mapping program in BC, created with Island Health and Provincial Health Services Authority.
That program had been years in the making but COVID kickstarted it. St. Paul’s CI audiologist Myron Huen says: “Creating partnerships like this provides seamless care for our patients. Technology like this enables patients to receive care closer to their homes, while connecting virtually makes it a smooth experience for both patient and health care provider.”
Research changes course
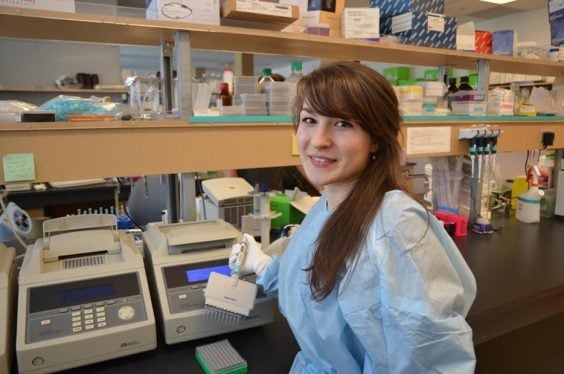
When the pandemic hit last March, most research activities at Providence Health Care and other institutions around the world were curtailed, with the exception of COVID-19 studies. Almost overnight, many researchers dropped their work and pivoted all their attention to SARS-CoV-2.
In the last year, researchers at Providence have collectively secured millions of dollars in COVID research funding. They’ve harnessed existing equipment and expertise to launch dozens of COVID-related studies – from diagnostic research to interventional clinical studies and community research.
The pace has been swift. Going from idea to publication to impacting patient care in a matter of months, rather than years, was previously unheard of in the world of health research. This is a testament to the incredible teamwork and collaborative partnerships formed across Providence and beyond.
COVID puts new electronic health system to the test

One year ago, 8,000 staff and medical staff across Providence Health Care’s acute sites had barely taken the training wheels off their new electronic health system, when the pandemic hit Vancouver. It was time to put the new system to the test.
Immediately, CST Cerner proved invaluable with the CST project team quickly able to add new pandemic functionality. This made it possible to access COVID-related information to build a multitude of real-time reports to help our Emergency Operations Centre, Operations Leaders, and IPAC team respond to the pandemic.
The electronic health record also made contract tracing in the hospital setting much easier. The system provides not only a record of patients who have tested positive, but a list of caregivers who saw the patient and may be at risk of contracting the virus.
The third major benefit was the ease of moving to a virtual health environment in CST Cerner. In particular, remote access allowed medical staff to manage electronic charts and use the same functionality that they were familiar with at the hospital, from home.
Although our remaining site implementations initially took a back seat to pandemic response planning, the project teams quickly adapted and made ground. Over the past nine months we have launched five successful implementations that brought additional ambulatory clinics, tertiary mental health units, assisted living and all of Providence’s long term care sites live on the system.
24/7 efforts help get COVID equipment to hospitals in need

For the Lower Mainland Biomedical Engineering team, there has been no more important COVID equipment than ventilators.
The Providence-employed team of technologists and engineers works within hospitals around the Lower Mainland, ensuring that medical technology – from monitors to MRI machines – supports patient care.
In the early days of the pandemic, this meant working around the clock to help prepare COVID units that were being set up at St. Paul’s Hospital and other major Lower Mainland hospitals. This included setting up monitors and ventilators, and sharing knowledge with clinical teams. As the pandemic continued, they refurbished and repaired an ongoing supply of the vital devices.
The pandemic has also gave the biomedical engineering team a chance to shine provincially. They currently manage a fleet of ventilators and they have securely shipped the devices across the BC. The biomedical engineering team is also supporting a provincial dashboard of ICU ventilator inventory and this data is used to help determine where to deploy needed ventilators.
St. Paul’s establishes first post-COVID-19 clinic

Months into the pandemic, some people who had contracted the virus noticed something alarming: they were still sick. The acute symptoms were lessening, but in their place were crushing fatigue, brain fog, shortness of breath and nausea. A colloquial term for this group arose: COVID “long-haulers.”
Health-care providers noticed more and more of these patients, too, and as a result, St. Paul’s opened a post-COVID clinic last year to care for these patients. Soon a network of these recovery clinics was formed, including St. Paul’, Vancouver General Hospital and the Jim Pattison Outpatient Care and Surgery Centre in Surrey.
The clinics provide care from numerous specialists – cardiologists, neurologists, psychologists, nurses, social workers and others – to let specialists understand the long-term adverse effects of COVID-19.
Research is a key component of this network to better inform clinicians as they continue to treat these patients.
Pandemic helps keep things “local” at Breast Clinic

Pre-pandemic, some anesthesiologists at the Providence Breast Centre at Mount Saint Joseph Hospital were using a regional nerve block on patients requiring surgery related to breast cancer.
When COVID-19 hit, the team quickly realized increased use of this technique, which involves local anesthetic, could bring a host of benefits.
For a general anesthetic, doctors must insert a breathing tube into the patient, increasing the risk of aerosol droplet exposure. For the nerve block, doctors inject a local anesthetic into the back and chest to numb the breast area. There is no loss of consciousness, paralysis, or a breathing tube.
The result: a lower risk of the virus’s transmission among Operating Room staff, reduced need for personal protective equipment, shorter hospital stays and increased capacity for breast surgeries.
Patients who have the block recover more quickly and report less pain after surgery than patients who receive a general anesthetic and fewer side effects.
Given the positives, clinic anesthesiologists will use this nerve block process more often, benefitting health-care workers and patients alike.
Existing technology helps diagnose COVID in remote, rural areas

When the pandemic struck, many infected British Columbians were showing respiratory symptoms – some severe. They needed an accurate diagnosis as quickly as possible to provide the best treatment.
This was difficult for those in rural and remote areas.
Fortunately, an innovation created before COVID as part of the federally funded Digital Technology Supercluster project would be a big help.
Accurate bedside diagnosis of lung disease related to COVID-19 is now accessible anywhere in BC through a network of portable handheld ultrasound scanners as part of the Supercluster project. The devices are paired with a cloud-based platform to create an ultrasound network to deliver fast, accurate diagnoses to patients.
This means rural and remote health care practitioners with limited access to specialists can now diagnose pneumonia from suspected COVID-19 patients in real time.
With this scanner, doctors can detect COVID-19 lung changes earlier while waiting for lab test results (the gold standard of diagnoses). They can anticipate who will likely deteriorate rapidly and support these patients early on.
The technology means BC patients, no matter where they live, now have equal access to life-saving ultrasound diagnoses and more accurate treatment.
Watch this video to learn more.





